Mast cells are regulators and protectors of the human immune system. By creating inflammatory and allergic responses, they play a powerful role in wound healing and help protect us from allergens, diseases and viruses.  Mast cells are key players in protecting the body but what happens when they no longer function as they should and the very cell meant to protect our lives becomes the one, which, inadvertently, begins to harm it. Idiopathic anaphylaxis, itching, flushing, migraines, bone pain, fatigue, cystitis; these are just a few of the unpleasant realities for patients suffering with the mast cell disorder, Mast Cell Activation Syndrome (MCAS).
Mast cells are key players in protecting the body but what happens when they no longer function as they should and the very cell meant to protect our lives becomes the one, which, inadvertently, begins to harm it. Idiopathic anaphylaxis, itching, flushing, migraines, bone pain, fatigue, cystitis; these are just a few of the unpleasant realities for patients suffering with the mast cell disorder, Mast Cell Activation Syndrome (MCAS).
What Are Mast Cells?
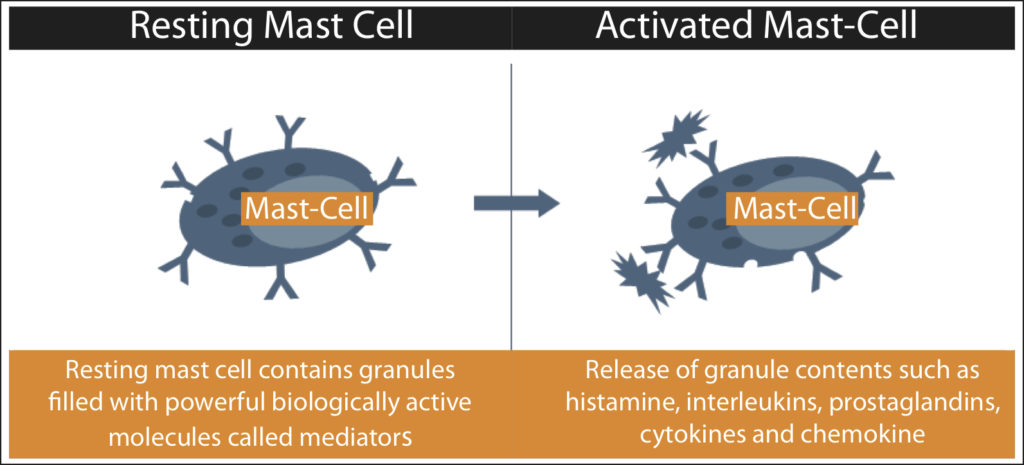
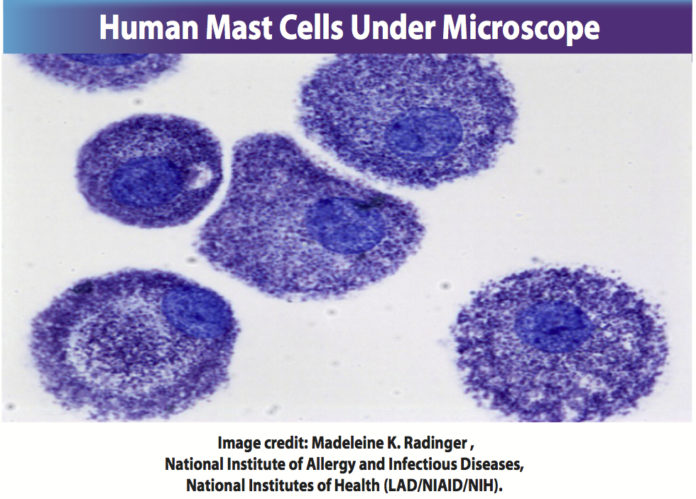
Mast cells are a type of white blood cell that originate in bone marrow and migrate through the blood to take up residence in tissues throughout the body. They are found most commonly between internal and external layers of tissues (lining bowels, skin). Mast cells are ideally placed to participate in the early recognition of pathogens or allergens. Mast cells are composed of storage sacks containing powerful biologically active molecules called mediators. When possible pathogens, allergens or threats are detected, mast cells become active and degranulate, secreting and releasing these powerful chemical mediators, which include histamine, interleukins, prostaglandins, cytokines and chemokine in an attempt to protect the body. The release of these chemicals causes inflammatory and allergic symptoms such as anaphylaxis, swelling, itching, hives, stomach cramps, heart palpitations, congestion, sneezing and can lead to complications involving every tissue and organ in the body.
What is Mast Cell Activation Syndrome?
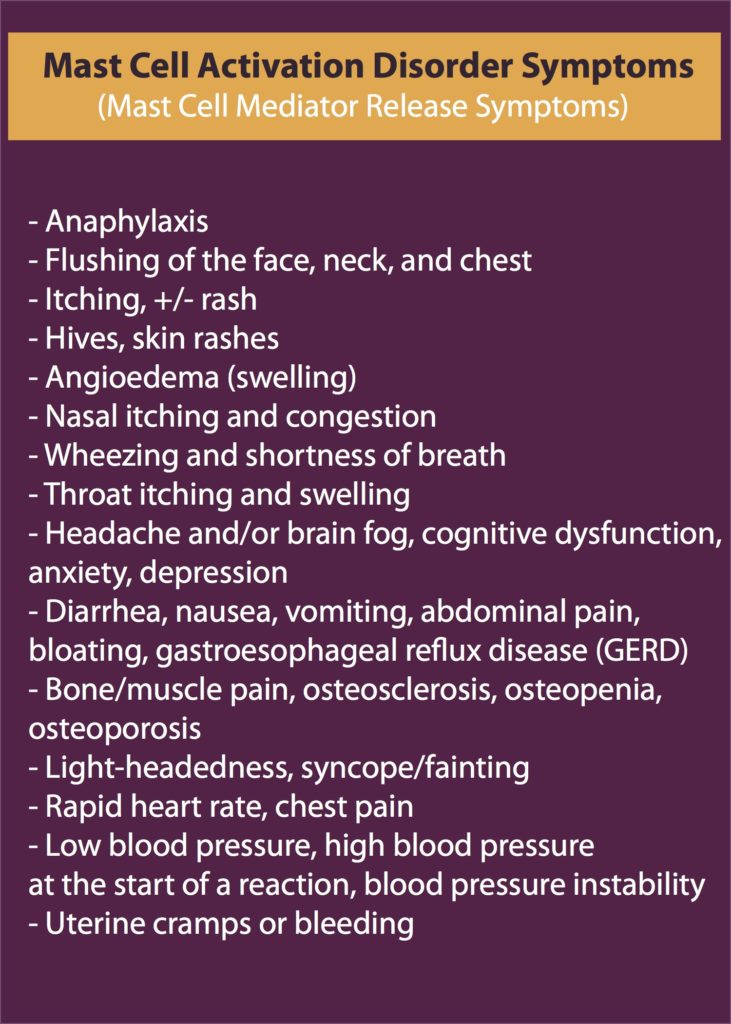
In the last decade, a mast cell disorder called Mast Cell Activation Syndrome (MCAS) has been identified. According to leaders in the field of MCAS, as much as 14%-17% of the population, or 1 of every 6-7 people, may be affected with this disorder. So could you or someone you love have MCAS? Individuals with MCAS have ongoing inflammatory and allergic symptoms such as anaphylaxis, hives, wheezing, digestive issues, bone pain, joint pain, and neurological issues (please see symptom chart below). These symptoms can flare up and come and go, or wax and wane over years. While other mast cell disorders can be attributed to oddly shaped or excessive numbers of mast cells, MCAS results from mast cells that are over-active and degranulating excessively, releasing histamine and other chemicals into the body on an unpredictable and ongoing basis. These chemicals, meant to alert the immune system to threat, release excessively in MCAS patients leading to ongoing inflammatory and allergic type symptoms in every tissue and organ of the body.
Symptoms
MCAS symptoms can involve the skin, gastrointestinal tract, cardiovascular, respiratory, and neurologic systems and can present as skin rashes, swelling, hives, wheezing, chest pain, dizziness, diarrhea, nausea, abdominal pain, headache, non-cardiac chest pain, tachycardia, neuropathic pain, joint and bone pain, insomnia, conjunctivitis, hypercholesterolemia, and elevated prostaglandin levels. Moreover, many diseases can be a result of ongoing and untreated MCAS in the body such as autism, autoimmune diseases, arthritis, cystitis, fibromyalgia, chronic migraine, osteoporosis, irritable bowel syndrome, anxiety, depression and chronic fatigue syndrome.
What Causes MCAS?
There is no known cause for MCAS and it is not contagious. Leading theories assert that it is likely acquired relatively early in life and may be the result of certain genetic mutations combined with environmental risk factors. Theories about genetic mutations abound as MCAS sufferers are often found in the same families. Moreover, environmental factors such as an intensely stressful emotional event or excessive stress on the body (accident, exposure to toxins) often precipitate the onset of MCAS symptoms. The overall consensus is that some individuals are genetically prone, whether through cell mutations or other means, to developing MCAS and when they are exposed to a stressful situation emotionally and/or physically, this disorder is triggered.
How is Mast Cell Activation Syndrome Diagnosed?
Mast Cell Activation Syndrome was first recognized in 1991 and finally given a name in 2007. MCAS is a disease that is difficult to diagnose. Prior to the discovery of MCAS, the more commonly known mast cell disorder was Systemic Mastocytosis. While those who suffer both MCAS and SM share the same inflammatory and allergic symptomology, the latter is easily identified with standard testing (biopsies, blood, urine, etc.). For an unknown reason, those who have MCAS often do not present with the tell tale genetic markers for mast cell dysfunction nor do they always test positive for the disease during blood and urine tests. However, such individuals continue to have life-altering or debilitating MCAS symptoms. Moreover, some people who have laboratory tests that are positive for MCAS live life symptom free. Another issue in diagnosing MCAS is that no two MCAS patients are alike. This is due to the fact that MCAS symptoms are vast in their presentation and can also involve any tissue or organ in the body. As a result, it is often hard to recognize a symptom or illness as being MCAS related. Causing even more confusion for MCAS diagnosis is that those who have this disorder usually experience a rise and fall in their symptoms throughout their lives, as well the remission of certain symptoms and the development of new symptoms. This waxing and waning makes MCAS an elusive disease, the usual time span from onset of symptoms to diagnosis being at least ten years.
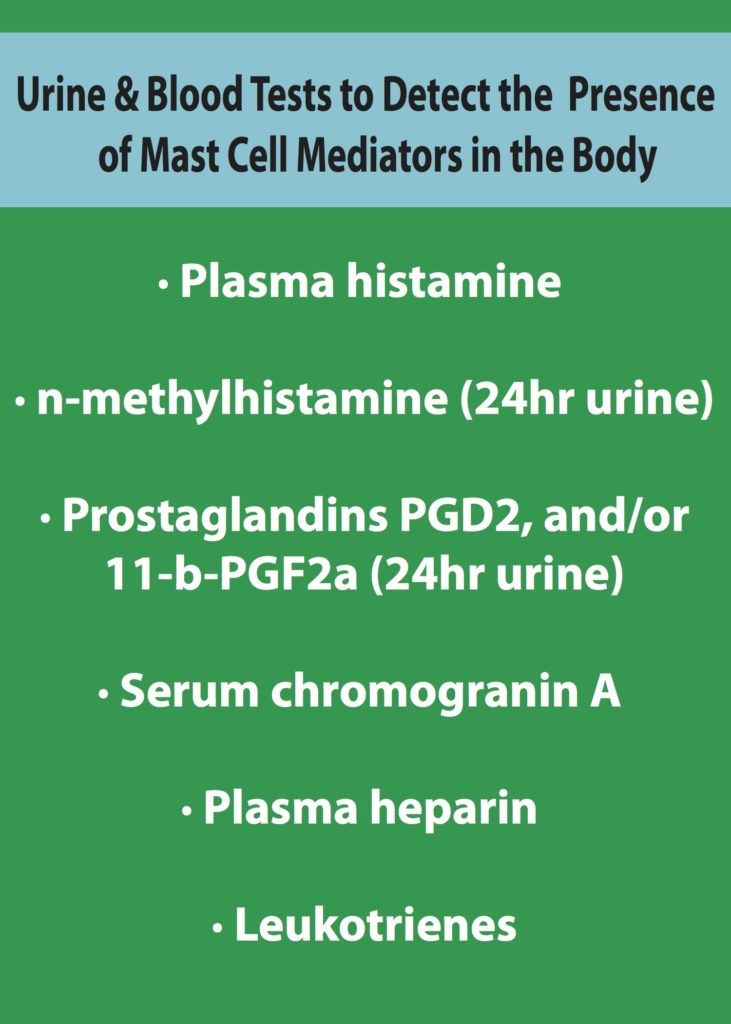
While MCAS is hard to diagnose, the good news is that forward thinking physicians are certain that this disorder can be diagnosed through thorough and meticulous clinical assessments, closely observing patient history and doing ongoing blood and urine testing. Such doctors are working hard to create awareness about MCAS and help define standardized diagnostic practices and criteria to diagnose this disorder more clearly and efficiently. By taking the time with a patient to learn their full symptomology and history, I believe that it is possible to diagnose MCAS accurately. Moreover, doing ongoing blood and urine tests which measure the presence of mast cell mediators in the body such as plasma histamine, n-methyl histamine (24hr urine), prostaglandins PGD2, and/or 11-b-PGF2a (24hr urine), serum chromogranin A, plasma heparin, and leukotrienes, help to give a clearer picture of the patient’s MCAS related symptoms and the state of their disorder. It is important that such blood tests continue on for a long period of time as mast cell mediators are not always identifiable if the patient’s mast cells are not currently being triggered. Though this approach can be laborious for physicians and patients, it is well worth the time. Research proves that clinical diagnosis and ongoing blood and urine testing are the only current surefire ways to determine whether someone has MCAS. It is an incredibly worthwhile pursuit to discover if a patient is suffering from MCAS. Treatment for this disorder often brings great relief and freedom to patients, and stops the progression of this disease and the other diseases it could cause.
Treating Mast Cell Activation Syndrome
The symptoms of MCAS can be greatly reduced through a mixture of traditional and natural treatments. Such treatments include: avoidance of triggers, use of antihistamines and mast cell stabilizing compounds and supplements, dietary restrictions and changes, and use of medications and supplements targeted at treating specific MCAS symptoms and complications.
Avoidance of MCAS Triggers
Each MCAS patient has a unique set of triggers that cause their mast cells to degranulate. These triggers are shared in common by many MCAS sufferers and include physical factors such as temperature changes, friction, exercise, fever, emotional stress, alcohol, drugs (NSAIDS, Opioids), chemicals, scents and high histamine foods. Some patients are susceptible to some or all of these well known mast cell triggers and they are well aware of them, while other patients do not seem to know what is triggering their mast cells to degranulate. The best way for a MCAS patient to identify and remember their triggers is to maintain an ongoing record, updating it as needed.
Traditional Anti-Histamines Used to Treat MCAS
H1 Blockers – hydroxyzine, doxepin, diphenhydramine (Benadryl), cetirizine (Reactine), loratadine (Claritin), fexofenadine.
H2 Blockers – Famotidine (Pepcid, Pepcid AC), Cimetidine (Tagamet, Tagamet HB), Ranitidine (Zantac)
Traditional Mast Cell Inhibitors and Stabilizing Compounds
Leukotriene inhibitors – Montelukast (Singulair), Zafirlukast (Accolate)
Mast cell stabilizers – Cromolyn, Ketotifen, Hyroxyurea, Tyrosine kinase inhibitors – imatinib
Natural Anti-Histamines and Mast-Cell Stabilizers
An exciting new development in MCAS research has been the discovery that Quercetin is more powerful than Cromolyn Sodium in blocking human mast cell cytokine release. MCAS specialists and patients are thrilled at this new development and many have begun to experience great symptom relief by supplementing with products that include this natural anti-histamine and mast cell stabilizer.
- Quercetin
- Ascorbic Acid
- Vitamin B6 (pyridoxal-5-phosphate)
- Omega-3 fatty acids (fish oil, krill oil)
- Alpha Lipoic Acid
- N-acetylcysteine (NAC)
- Methylation donors (SAMe, B12, methyl-folate, riboflavin)
- Certain probiotics decrease histamine production
- Lactobacillus rhamnosus and bifidobacter species
- DAO enzymes with meals – UmbrelluxDAO
Low Histamine Diet
The low histamine diet can seem challenging to follow but for some MCAS patients, it spells great relief. Key to succeeding on this diet is the avoidance of high histamine or histamine releasing foods such as:
- Alcoholic beverages
- Raw and cured sausage products such as salami.
- Processed or smoked fish products. Use freshly caught seafood instead.
- Pickles
- Citrus fruits
- Chocolate
- Nuts
- Products made with yeast and yeast extracts
- Soy sauce and fermented soy products
- Black tea and instant coffee
- Aged cheese
- Spinach (in large quantities)
- Tomatoes, ketchup and tomato sauces
- Artificial food colorings & preservatives
- Certain spices: cinnamon, chili powder, cloves, anise, nutmeg, curry powder, cayenne pepper
- Food additives such as MSG, Sulphites
Introduction of Anti-Histamine Foods
There are delicious foods with powerful anti-histamine qualities such apples, peaches, turmeric, garlic and watercress. For many MCAS patients, adding these foods to their diet makes a big difference in symptom control and quality of life. Please refer to the chart below for a full listing of these foods.
MCAS Traditional and Natural Symptom Management
Headaches can be treated with paracetamol, metamizole, flupirtine, ginger (natural)
Diarrhea can be treated with colestyramine, nystatin, montelukast, ondansetron, probiotics (natural), prebiotic fiber (natural)
Abdominal pain can be treated with metamizole, butylscopolamine, ginger (natural)
Nausea can be treated with metoclopramide, dimenhydrinate, icatibant, ginger, fresh lemon in cold water (natural)
Respiratory symptoms (phlegm) can be treated with montelukast, acute/short-acting albuterol, steam inhalation (natural)
Gastric complaints can be treated with proton pump inhibitors, walking Osteoporosis/bone pain can be treated with biphosphonates, Vitamin D plus calcium (natural)
Joint pain can be treated with omega oils (natural)
Non-cardiac chest pain can be treated with H2-histamine receptor antagonist, proton pump inhibitors
Tachycardia can be treated with verapamil; AT1-receptor antagonists; ivabradin
Neuropathies can be treated with a-lipoic acid (natural)
Interstitial cystitis can be treated with pentosan, D-Mannose (natural), avoidance of alcohol, caffeine, citrus
Sleep-onset insomnia/sleep-maintenance insomnia can be treated with triazolam, oxazepam, melatonin (natural), tryptophan (natural)
Conjunctivitis can be treated with drops containing glucocorticoids
Looking to the Future for Mast Cell Activation Syndrome Patients
Mast Cell Activation Syndrome is a potentially life altering disorder with a very diverse symptomology. It can cause symptoms in every tissue and organ of the body, ranging from slightly uncomfortable (headache) to debilitating and possibly deadly (anaphylaxis). Many individuals who suffer from MCAS have a host of MCAS symptoms, as well as other diseases as a result of their overactive mast cells releasing histamine and other powerful chemicals into their bodies and causing inflammatory and allergic processes. In the last 10 years, the medical community has begun to recognize that MCAS sufferers abound and new diagnostic approaches and effective treatments are coming to the aid of such individuals. Through effective diagnosis and simple treatments, MCAS patients the world over are getting their lives back. The life altering symptoms and diseases that result from MCAS can be managed and stopped through traditional and natural treatments, education and lifestyle changes. If you think MCAS might be at the root of your symptoms or chronic health issues I encourage you to take action today by speaking to your doctor or sending me a message and taking steps towards making the medicinal, supplement and lifestyle changes needed to live your life symptom free. I utilize a customized treatment plan for each patient, based on your unique triggers, lab findings, and lifestyle.
References
- Gilfillan AM, Austin SJ, Metcalfe DD. Mast cell biology: introduction and overview. Adv Exp Med Biol. 2011;716:2-12. http://www.ncbi.nlm.nih.gov/pubmed/21713648
- Theoharides TC, Valent P, Akin C. Mast Cells, Mastocytosis, and Related Disorders. N Engl J Med. 2015 Jul 9;373(2):163-72. http://www.ncbi.nlm.nih.gov/pubmed/26154789
- Afrin LB. Presentation, diagnosis and management of mast cell activation syndrome. In: Murray DB, editor. Mast cells: phenotypic features, biological functions and role in immunity. Hauppauge: Nova Science Publishers, Inc.; 2013. p. 155-232.
- Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157(3):215-25. http://www.ncbi.nlm.nih.gov/pubmed/22041891
- Akin C, Scott LM, Kocabas CN, Kushnir-Sukhov N, Brittain E, Noel P, et al. Demonstration of an aberrant mast-cell population with clonal markers in a subset of patients with “idiopathic” anaphylaxis. Blood. 2007 Oct 1;110(7):2331-3. http://www.ncbi.nlm.nih.gov/pubmed/17638853
- Horny HP, Sotlar K, Valent P. Evaluation of mast cell activation syndromes: impact of pathology and immunohistology. Int Arch Allergy Immunol. 2012;159(1):1-5. http://www.ncbi.nlm.nih.gov/pubmed/22555026
- Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013 Apr;68(4):417-24. http://www.ncbi.nlm.nih.gov/pubmed/23409940
- A, Fu X, Katsarou-Katsari A, Antoniou C, Theoharides TC. Quercetin is more effective than cromolyn in blocking human mast cell cytokine release and inhibits contact dermatitis and photosensitivity in humans. PLOS ONE. 2012 Mar;7(3). http://journals.plos.org/plosone/article/related?id=10.1371/journal.pone.0033805








Good Morning Dr. Maxwell,
I just read that exercise may be a trigger. My 11 year old daughter was just diagnosed with MCAS for very elevated prostaglandin levels. I have had her in physical therapy and now wondering if I should stop it. She comes out telling me how terrible she feels. I just want to double check that exercise can in fact cause a reaction with her mast cells?
This is an awful disease. Thank you for taking this research on.
Hello Suzanne,
Thank you for contacting me. I certainly understand your anxiety and frustration regarding your daughter’s recent diagnosis. The good news is that there is much that can be done
to help MCAS!
Unfortunately, exercise can be a trigger for MCAS in some individuals. As each patient is unique as to what can trigger their MCAS, I often recommend easing into exercise to find what each patient’s tolerance
level is. In general, getting overheated during exercise is best to avoid. In my experience, as exercise endurance improves, there is a declining chance of MCAS activation.
Please keep me posted on your daughter’s progress!
Warmest regards,
Dr. Maxwell
Thank You so much!
How can I set up an appt. To meet with you. I have 95% if the above symptoms for over eight years now. I am fine for a couple months then..WHAM! It has progressively gotten worse and no body seems to understand what’s going on…not even a hematologist that I’ve been seeing for iron infusions.
Hi Brenda,
I am sorry to hear about your symptoms. Please give my office a call at 513-741-4404. We will be glad to answer any questions you may have, and schedule a consultation with you.
Warmest regards,
Dr. Maxwell
Hello, for the past 10 years, after my Iraq tour I have had episodes of swelling that last multiple days. It went away for a few years and seems to be back.
I noticed if I have a rough/long couple days and have extra caffeine, I get swelling on each lip sepereatley, followed by my jaw. The swelling changes my entire face.
Just yesterday I went to a concert and we drank alcohol, and got home late. On these occasions the swelling and itching starts on my feet, moves to my left bicep, then hands and then each lip and cheeks and finally each side of tongue. This can literally last a few days to a week as it runs its course.
Where do I go to get diagnosed in North Jersey? Does this sound like it can be Mast Cell?
I also have had tons of gas and bloating.
Thank you very much!
Hello Rob,
First of all, thank you for your service!
I feel the best way to help you is through a telemedicine (phone) consultation. This includes a complete review of your medical history, any test results, and consultations. Further testing can be ordered, if needed. My goal is to find, and treat, any underlying cause(s). A customized treatment plan is then recommended.
Please contact my nurse, Debra, through drcraigmaxwell@roadrunner.com. She will be glad to assist you and answer any questions you have.
I look forward to helping you, Rob!
Warmest regards,
Dr. Maxwell
Very good information.
Thank you